When It Happens to One of Us: Vicarious Trauma and the Monash IVF Embryo Error
By Elizabeth Bancroft, Clinical & Counselling Psychologist | Founder, Hope Affirm Thrive
In June 2025, Monash IVF confirmed a deeply troubling error: during a fertility treatment, the patient's own embryo was used instead of their partner’s, contrary to the agreed-upon treatment plan. The company publicly acknowledged the mistake, which it attributed to a "human error" in embryo identification and handling.
This is not the first time this has happened.
Earlier this year, Monash IVF admitted to another embryo mix-up—one that resulted in a couple carrying a pregnancy from an embryo not genetically related to them at all.
Two errors. One year. One fertility provider.
For thousands of IVF patients across Australia, this news didn’t just trigger outrage—it triggered trauma. Even those not directly involved in either incident found themselves overwhelmed by fear, uncertainty, and grief.
This is known as vicarious trauma—and it’s time we talked about it.
What Is Vicarious Trauma?
Vicarious trauma is the emotional and physiological response we experience when exposed to someone else’s traumatic story, especially when it mirrors a fear or experience we’ve personally lived. While it’s often discussed in the context of therapists or emergency responders, medical patients are not immune.
According to the American Counseling Association, vicarious trauma can alter a person’s sense of safety, control, trust, and meaning—especially in systems where power is already unequal and uncertainty is constant.
In fertility care, the connection is visceral. Whether you’ve completed treatment, are in the thick of it, or are still considering IVF, news like this hits you somewhere deep. You start asking:
What if that had been my embryo?
Can I really trust the system I’ve already handed so much over to?
How would I even know if something went wrong in my case?
This isn’t catastrophizing. It’s a trauma response—particularly common in systems where patients must surrender control and rely on professionals to safeguard something as precious as genetic material.
Why This Error Feels So Personal
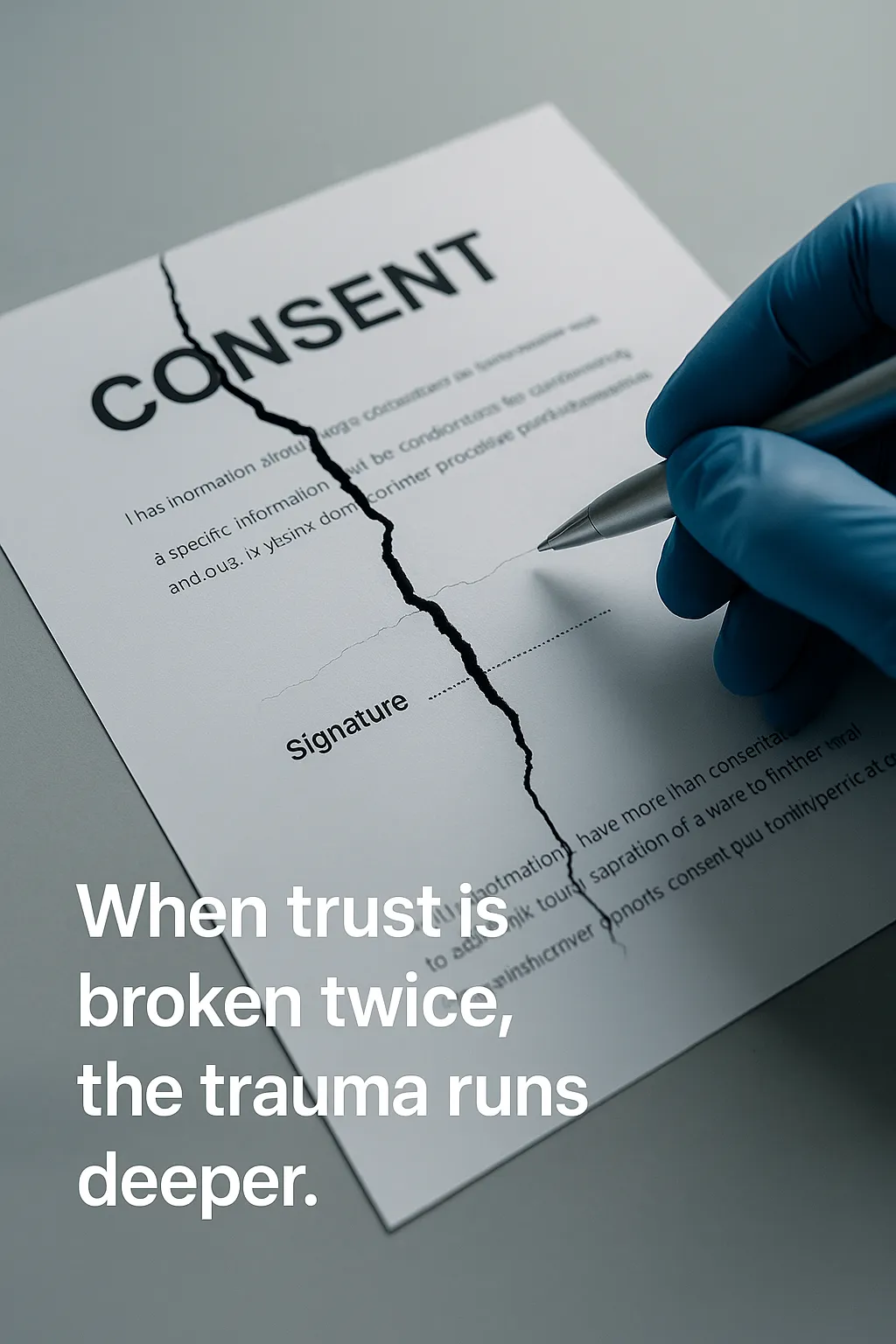
IVF patients already live with uncertainty. Even when everything goes “right,” the stakes are enormous and the emotional load is heavy. But what makes this incident (and the one earlier this year) so psychologically destabilising is the breach of trust.
So when Monash IVF confirms two separate embryo bungles in the same year, it ruptures something far deeper than policy—it shakes the very foundation of patient trust.
And for many, it reactivates trauma they thought they’d buried:
🔹 The uncertainty of embryo survival
🔹 The grief of failed transfers
🔹 The fear that something went wrong that they were never told
These aren't paranoid thoughts. They’re trauma echoes.
This latest bungle—using the wrong embryo, even if it was the patient’s own—also represents more than a deviation from protocol. It raises alarming questions:
Was the consent process robust enough?
How did this mistake bypass safety checks?
Could something similar have happened to me, and I’d never know?
For many, these are not theoretical fears. IVF patients routinely report medical anxiety, hypervigilance, and feelings of powerlessness, even without these kinds of scandals. When the system falters twice in one year, it creates a sense of systemic instability that patients can't just shrug off.
The Compounding Effect: Two Errors, One Systemic Impact
This isn’t a one-off anomaly. Two confirmed embryo misidentifications in a single calendar year—both from the same institution—suggest deeper cracks in the system.
Psychologically, this compounds trauma in three key ways:
Reinforcement of danger: When a system fails twice, it shifts from “freak accident” to perceived pattern.
Loss of illusion of safety: IVF is already emotionally and physically taxing. Patients rely on the belief that their embryos are safe. That belief is now broken.
Widening of the trauma net: The more frequent the errors, the more patients see themselves in the headlines.
This cumulative effect is well-documented in trauma literature. When breaches of trust happen in succession, the nervous system remains on high alert, with less and less capacity to return to baseline. This is especially true for those with pre-existing anxiety, PTSD, or medical trauma.
Psychologist Jennifer Freyd’s research on institutional betrayal explains how trauma is magnified when an institution someone relies on for safety fails them—or someone like them. That betrayal is especially potent when the stakes involve bodily autonomy, consent, and family creation.
For IVF patients, two embryo errors in a single year doesn’t feel like isolated incidents. It feels like evidence that the system is not as safe or careful as promised. And that’s enough to retraumatise patients who thought their story was finished.
Who Is Most at Risk?
While anyone who’s been through fertility treatment may be affected by this news, certain groups are especially vulnerable:
Neurodivergent patients, who often rely on clear protocols and struggle more with uncertainty and disrupted trust
Those with prior medical trauma, including previous IVF losses or miscommunications with providers
People currently in treatment, for whom this news directly undermines their present-day care
Highly sensitive or empathic individuals, who may experience the trauma in their own bodies
Research on Medical Betrayal and IVF Distress
Smith & Freyd (2014) describe institutional betrayal trauma as what happens when an organization we depend on for safety—like a hospital or fertility clinic—violates that trust. It can trigger dissociation, hypervigilance, and long-term mistrust in healthcare systems.
A 2019 systematic review published in Human Reproduction Update found that distress in fertility patients is significantly increased when there’s a lack of transparency and poor communication from providers.
Neurodivergent and highly sensitive patients may be even more vulnerable. A 2023 meta-analysis noted elevated trauma responses in autistic and ADHD individuals undergoing complex medical procedures, especially where systems lacked predictability and patient-centered communication.
What You’re Feeling Is Valid
If you're feeling:
Distrustful of your fertility clinic
Hyperaware of every decision made in your case
Emotionally flooded or retraumatised
Angry, scared, or numb
…it’s not because you’re overreacting. It’s because this is terrifying—and it’s happened twice this year in a system we’re all told to trust with our family’s future.
Where Do We Go From Here?
The fertility industry must be held accountable—not only for procedural safety, but for the emotional and psychological duty of care owed to patients.
Patients deserve:
🔸 Transparent reporting of errors
🔸 Independent regulatory oversight
🔸 A trauma-informed approach that acknowledges the real mental health toll of fertility care
And if you're still carrying the weight of this story in your body, you’re not alone. Whether you're between cycles, pregnant after IVF, or quietly closing the chapter on fertility treatment, you deserve support to process what this news brings up.
This Is Why Trauma-Informed IVF Support Exists
At Hope Affirm Thrive, we support patients through the emotional terrain of IVF—from fear and burnout to post-treatment grief and trauma recovery. These news stories are part of that terrain. And we take them seriously.
Because when a clinic makes the same mistake twice in a year, it’s no longer a fluke.
And when it happens to one of us—it happens to all of us.
References
1. Gameiro, S. et al. (2019). "Psychosocial adjustment in patients undergoing fertility treatment: A systematic review." Human Reproduction Update.
2. Smith, C. & Freyd, J. J. (2014). "Institutional betrayal." American Psychologist.
3. Duvekot, J. et al. (2023). "Neurodivergence, trauma sensitivity, and medical care: a meta-analysis." Journal of Psychosomatic Research.
4. Pearlman, L. & Saakvitne, K. W. (1995). Trauma and the Therapist: Countertransference and Vicarious Traumatization
