
The IVF Industry Has a Blind Spot: Trauma and Neurodivergence
Title: The IVF Industry Has a Blind Spot: Trauma and Neurodivergence
By Liz Bancroft
When I walked into the fertility clinic for my first egg collection, I had no idea I would leave feeling more broken than hopeful. I was a psychologist, a new patient, and a woman who had spent years helping others recover from trauma. Yet on that day, I found myself shut down, overwhelmed, and invisible in a system that treats infertility as purely a medical problem, rather than a human one.
What I experienced wasn’t a fluke. It was a consequence of a system that consistently overlooks how trauma history and neurodivergent brains interact with the demands of fertility treatment. And the consequences aren’t just emotional—they may be physiological, too.
We now know that chronic stress and trauma-related dysregulation can interfere with reproductive outcomes. Research has begun to link cortisol levels, nervous system activation, and emotional distress to egg quality, embryo development, and implantation success. And yet, most fertility clinics do little to identify or support patients experiencing these very real barriers.
Here’s what that looks like in real life:
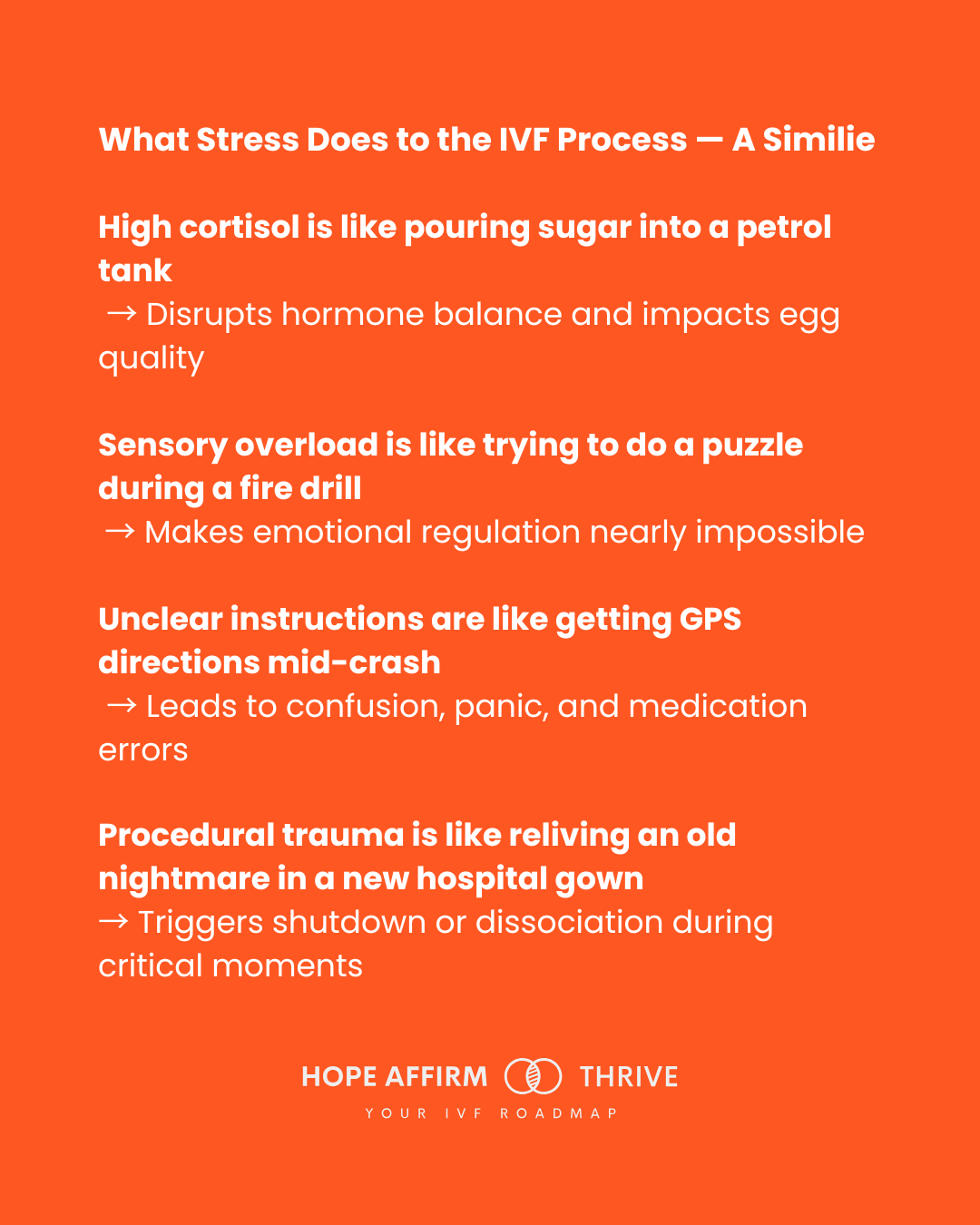
Stress isn’t just a feeling—it’s a full-body disruption. Here’s how trauma and neurodivergence can interfere with IVF at every step, using everyday metaphors to make the science stick.
As both a psychologist and an autistic woman, I have a front-row seat to this problem. In my practice, I support many neurodivergent women attempting IVF, and the patterns are striking. Their experiences are consistently more stressful, less supported, and more misunderstood. These women often arrive in the fertility system already carrying the psychological weight of being different. Many are late-diagnosed, highly intelligent, and have spent years masking their distress to fit into systems not designed for them.
Fertility treatment magnifies these challenges. The sensory environment of clinics—bright lights, strong smells, long wait times, and invasive procedures—can easily trigger sensory overload. Communication is another barrier: phone calls with last-minute changes, unclear medication instructions, rushed consultations. For someone with a neurodivergent brain, predictability is not just a preference; it’s a coping strategy. When that predictability is disrupted, so is their ability to function.
This isn’t just an inconvenience. It’s a health equity issue. If a certain subset of patients consistently experiences higher stress, lower trust in providers, and less emotional regulation during procedures like egg retrieval, then their outcomes may suffer through no fault of their own.
Trauma complicates this further. Many neurodivergent women have trauma histories—medical, relational, or systemic. IVF can re-activate these wounds. Being sedated for a procedure while vulnerable and exposed, with limited control, may resemble dynamics of past abuse. Without trauma-informed care, the very process meant to help them build a family can become re-traumatising.
The irony is that these women are among the most prepared patients I know. They come with spreadsheets, carefully researched questions, and an almost superhuman capacity for emotional endurance. But that preparation is often misunderstood as controlling or rigid. Instead of being seen as a strength, it’s pathologised.
The solution is not more mindfulness apps and wellness coaches. It’s a systemic shift toward trauma-informed, neurodivergent-affirming reproductive care. Clinics need to screen for trauma and neurodivergence the same way they do for hormone levels. Staff need training to understand how dysregulation manifests, and how to offer communication and procedural accommodations that support nervous system safety.
Written instructions. Predictable routines. Sensory-friendly environments. Psychological safety protocols for high-anxiety procedures. These are not luxury add-ons. They are essential tools for equity in reproductive health.
Infertility is already an emotionally grueling experience. For those who carry the added burden of trauma and neurodivergence, it becomes a gauntlet. If we continue to ignore the role of the nervous system in fertility, we are not practicing medicine—we are practicing omission.
We owe our patients more. We owe them care that sees the whole person, not just their ovaries.
If you’re navigating IVF and feeling unseen or overstimulated by the process, you’re not alone—and you’re not too much. My work at Hope Affirm Thrive is built for people like you.
Learn more about how we support neurodivergent women through IVF.
---
References
Anifandis, G., et al. (2015). The impact of stress on fertility, hormonal function, and IVF success rates. Journal of Reproductive Biology and Endocrinology.
Rooney, K. L., & Domar, A. D. (2018). The relationship between stress and infertility. Dialogues in Clinical Neuroscience.
Crane, L., et al. (2021). Autistic people’s experiences of healthcare: A systematic review of studies. BMJ Open.
Raymaker, D., et al. (2017). Prevalence of trauma in autistic adults. Autism in Adulthood.
Courtois, C. A., & Ford, J. D. (2013). Treatment of Complex Trauma: A Sequenced, Relationship-Based Approach.
SAMHSA. (2014). Trauma-Informed Care in Behavioral Health Services.
Milton, D. (2012). The double empathy problem. Autism, 19(6), 774–782.
