PMDD: The Hidden Condition That Could Impact Your IVF Journey
PMDD: The Hidden Condition That Could Impact Your IVF Journey
What every woman should know about Premenstrual Dysphoric Disorder before starting fertility treatment
Starting your IVF journey is both exciting and overwhelming. You've likely researched success rates, lifestyle changes, and treatment protocols extensively. But there's one crucial factor that often flies under the radar: Premenstrual Dysphoric Disorder (PMDD). This serious hormonal condition affects millions of women worldwide and could significantly impact your fertility treatment experience.
Understanding PMDD before you begin IVF isn't just helpful—it's essential for optimizing your treatment outcomes and protecting your mental health during this vulnerable time.
What Is PMDD?
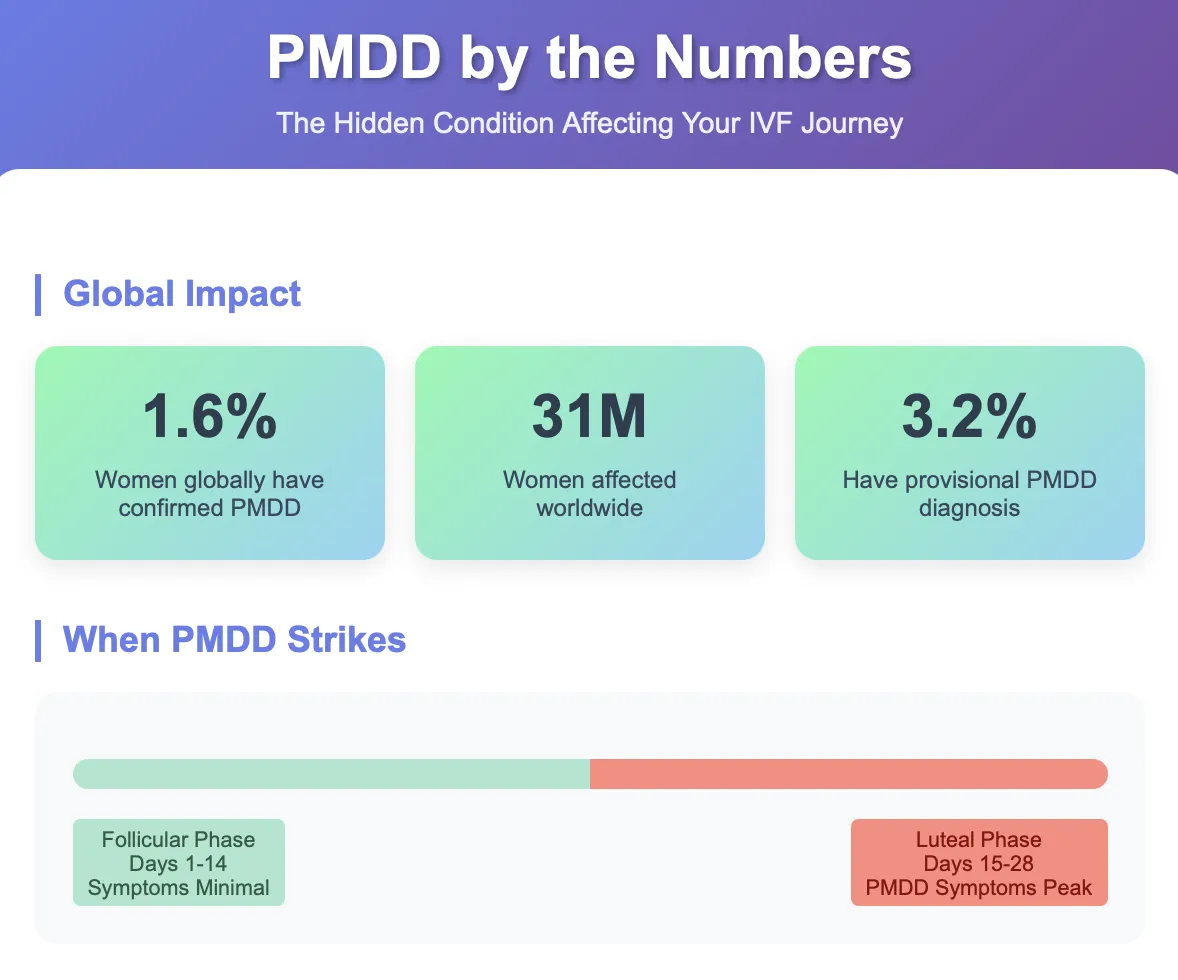
Premenstrual Dysphoric Disorder is far more than severe PMS. PMDD is a severe form of premenstrual syndrome that affects 5% to 8% of women of reproductive age, causing moderate-to-severe symptoms that can cause significant distress and functional impairment. Recent research published in the Journal of Affective Disorders provides even more precise figures: around 1.6% of women and girls have confirmed symptomatic PMDD, equivalent to around 31 million women and girls globally, with a higher proportion of 3.2% having provisional diagnoses.
PMDD is characterized by depressive mood, anxiety, mood liability, and somatic symptoms that usually appear during the late luteal phase of the menstrual cycle and typically disappear during the first week after menses. This isn't simply feeling moody before your period—it's a debilitating condition that can severely impact your ability to function in relationships, work, and daily life.
The Science Behind PMDD
The exact link between PMDD and hormonal fluctuations is still unknown, however evidence suggests that it does not necessarily result from any hormonal imbalance or dysfunction. In fact, the majority of women diagnosed with PMDD have normal hormone levels. Instead, PMDD results from hyper-sensitivity to the cyclical changes in the reproductive hormones oestrogen and progesterone, the latter in particular.
Research has demonstrated that the change in estradiol/progesterone levels from low to high, and not the steady-state level, was associated with onset of PMDD symptoms. This finding is crucial for understanding why IVF medications might affect women with PMDD differently.
How Do I Know If I Have PMDD?
Many women suffer with PMDD for years without a proper diagnosis. 19 out of 32 participants in a recent study self-diagnosed, with 17 of whom later receiving official diagnoses from providers. This highlights the importance of self-advocacy and awareness.
Key Symptoms to Watch For
According to the DSM-5 criteria, PMDD requires at least 5 of the following 11 symptoms (including at least 1 of the first 4 listed): markedly depressed mood, feelings of hopelessness, or self-deprecating thoughts; marked anxiety, tension, feelings of being "keyed up" or "on edge"; marked affective lability; marked anger or irritability; decreased interest in usual activities; difficulty concentrating; fatigue; appetite changes; sleep disturbances; feeling overwhelmed; and physical symptoms like breast tenderness, bloating, headaches, or joint pain.
The crucial differentiator: These symptoms must occur specifically during the luteal phase (the two weeks before your period) and resolve within a few days after menstruation begins. To diagnose PMDD, over the course of a year, during most menstrual cycles, you must have 5 or more symptoms that have been present during the week before your period and stopping within a few days after your period starts.
Getting a Proper Diagnosis
Your provider may ask that you keep a journal or diary of your symptoms for several months. This symptom tracking is essential for distinguishing PMDD from other mood disorders. In order to distinguish PMDD from a mental health disorder such as chronic depression or bipolar disorder, it is useful to keep a diary of symptoms over the course of a few menstrual cycles. By tracking your symptoms, it can demonstrate whether it is linked to a specific phase of your cycle.
The Serious Mental Health Impact
PMDD isn't just physically uncomfortable—it poses serious mental health risks. A global study of a sample of people diagnosed with PMDD revealed alarming statistics: 72% of participants had experienced suicidal ideation, 49% had made suicide plans, and 34% had attempted suicide.
There is little training around PMDD for psychiatrists or indeed medical students. Patients often find themselves falling through gaps in clinical services, such as between gynaecology and mental health services. This lack of awareness in the medical community makes self-education and advocacy even more critical.
The ADHD and Autism Connection: A Critical Link
One of the most significant but under-recognized aspects of PMDD is its disproportionate impact on neurodivergent individuals, particularly those with ADHD and autism. Recent groundbreaking research has revealed striking connections that every woman considering fertility treatment should understand.
ADHD and PMDD: The numbers are staggering. Research published in the British Journal of Psychiatry in 2025 found that the prevalence of provisional PMDD was elevated among individuals with a self-reported clinical ADHD diagnosis (31.4%), and among participants with ASRS-based ADHD (41.1%), compared with the non-ADHD reference group (9.8%). Even more concerning, individuals with ASRS-based ADHD and depression and/or anxiety diagnoses were at highest risk for provisional PMDD (relative risk 4.53 [3.10, 6.61]) compared with the non-ADHD reference group.
Autism and PMDD: The relationship with autism is equally significant. Studies suggest that up to 92% of autistic women and 46% of women with ADHD experience PMDD, though estimates vary. Other research shows that the prevalence of PMDD in autistic women ranges from 14.5% to 92%, with autistic women with learning disabilities being particularly susceptible, with 92% experiencing late luteal phase dysphoric disorder compared to 11% of non-autistic women with learning disabilities.
Why This Matters for Fertility Treatment: The intersection of these conditions creates unique challenges:
Hormone Sensitivity: As people with ADHD have reduced dopamine levels across the brain, hormone fluctuations may be more likely to reduce dopamine to critically low levels, leading to more severe feelings of exhaustion, moodiness, and lack of motivation
Sensory Processing: Autistic people generally have greater sensory sensitivity, and therefore may be more likely to be negatively affected by menses-related symptoms
Masked Symptoms: Females with Autism often have a different presentation to males with the diagnosis, which can again result in underdiagnosis or misdiagnosis. Females are more likely to engage in masking and the mimicking of social behaviours in an attempt to fit in
Clinical Implications: Clinicians should be aware that individuals with a diagnosis of ADHD, or with high ADHD symptom levels, and who have a menstrual cycle may be more likely to experience PMDD. This is particularly crucial during IVF, when hormonal fluctuations are dramatically amplified.

How PMDD Could Impact Your IVF Journey
Hormonal Sensitivity and Treatment Response
Here's where PMDD becomes particularly relevant to your fertility journey. IVF involves significant hormonal manipulation, and women with PMS/PMDD have a heightened sensitivity to cyclical variations in levels of reproductive hormones, which predisposes them to experience mood, behavioral, and somatic symptoms.
The hormonal medications used in IVF—including estrogen and progesterone supplementation—could potentially trigger or worsen PMDD symptoms. PMDD symptoms are eliminated by ovarian suppression and stimulated by administration of ovarian steroids, meaning that the very hormones used to optimize your fertility treatment might exacerbate your symptoms.
Medication Interactions and Treatment Conflicts
The more likely scenario is that your fertility is affected by the medication commonly prescribed to manage the symptoms of PMDD, such as the birth control pill or SSRIs. Certain treatments, particularly hormonal therapies like the contraceptive pill, disrupt the menstrual cycle by suppressing ovulation. If ovulation is suppressed, it is not possible to get pregnant.
This creates a complex situation: many first-line PMDD treatments involve suppressing ovulation, which directly conflicts with fertility goals. If you are trying to conceive, it's important to discuss these implications with your GP or healthcare specialist so that you are aware of any risks of changing your medication regime.
Stress and IVF Outcomes
Most studies concluded that stress has a negative effect on IVF treatment. The egg retrieval time point was most affected by chronic and acute stress. Given that PMDD can cause severe emotional distress, managing these symptoms becomes crucial for optimizing treatment outcomes.
Indirect Effects on Fertility
While there is no evidence to suggest PMDD and infertility are connected directly, the emotional and physical symptoms of PMDD can make you not feel like having sex as often, and that can affect your chances of getting pregnant. Some studies even suggest that women with PMDD might have irregular ovulation patterns, which can mess with their fertility windows.
Why Addressing PMDD Before IVF Is Critical
1. Treatment Planning and Medication Management
Understanding your PMDD status allows your fertility team to:
Modify hormonal protocols to minimize symptom exacerbation
Plan for potential mood changes during treatment
Coordinate care between reproductive endocrinologists and mental health professionals
If abnormally low progesterone levels are associated with PMDD, progesterone can be supplemented with medication during the course of Intrauterine Insemination or IVF treatment
2. Mental Health Support
ART itself has been shown in other studies to negatively impact a patient's psychological well-being, with prolonged treatment associated with increased depression and anxiety. For women with PMDD, this risk may be even higher, making proactive mental health support essential.
3. Optimizing Treatment Outcomes
Early intervention: Seeking medical guidance promptly upon symptom recognition. Adherence to advised treatments and protocols can make a significant difference in both PMDD management and fertility outcomes.
Treatment Options That Work With Fertility Goals
Non-Hormonal Approaches
Several evidence-based treatments can help manage PMDD without interfering with fertility:
Selective Serotonin Reuptake Inhibitors (SSRIs): Antidepressants that predominantly affect noradrenergic transmission are not as effective for PMDD as SRIs, which means that the effect of SRIs in PMDD is not just an antidepressant effect. This is supported by the fact that the beneficial effect of SRIs begins rapidly in PMDD, whereas antidepressant effect takes several weeks. Thus, clinicians can use SRIs intermittently from mid-cycle to menses to treat symptoms of PMDD as opposed to continuous treatment.
Lifestyle Interventions: Regular exercises, walking, or even yoga. Nutritious diet: Incorporating vitamin-rich foods and adequate hydration. Stress relief: Meditation, mindfulness exercises, and breathing techniques. Sleep routine: Ensuring 7-9 hours of restful sleep.
Innovative Treatments
Recently, a clinically significant reduction in the severity of the mental symptoms of PMDD was observed upon treatment with a selective progesterone receptor modulator (SPRM), as demonstrated when comparing ulipristal acetate with placebo in a randomised controlled trial. While these treatments are still being researched, they represent promising options for the future.
Therapy and Support
A 2024 study found that therapy can effectively help people manage common PMDD symptoms. Women in the EFT group showed significant improvement in emotion regulation and PMDD symptoms. Depression and stress levels also decreased.
Taking Action: Your Next Steps
1. Start Symptom Tracking Now
Begin keeping a detailed symptom diary for at least two cycles before starting IVF. Track:
Daily mood symptoms (1-10 scale)
Physical symptoms
Sleep patterns
Relationship impacts
Work/daily functioning
2. Assess Neurodivergent Status
Given the strong correlation between PMDD and neurodivergent conditions, consider whether you might have undiagnosed ADHD or autism. Many women receive these diagnoses for the first time during their reproductive years, often triggered by fertility struggles or hormonal changes. Key indicators include:
ADHD symptoms: Difficulty with attention, organization, time management, emotional regulation, and rejection sensitivity that worsen premenstrually
Autism traits: Sensory sensitivities, need for routine, social communication differences, intense interests, and increased masking behaviors during hormonal fluctuations
If you suspect you might be neurodivergent, seeking evaluation before IVF can help your healthcare team develop more targeted treatment strategies.
3. Seek Proper Diagnosis
Don't wait until you're in the middle of IVF treatment to address potential PMDD. The data emphasises that at a given timepoint there is still a significant minority of women with symptomatic PMDD, which is strongly associated with suicidal thoughts. Professional evaluation is crucial, especially if you have ADHD or autism traits.
4. Build Your Support Team
Consider assembling a care team that includes:
A reproductive endocrinologist familiar with PMDD and neurodivergent conditions
A psychiatrist or psychologist experienced in women's hormonal health and neurodiversity
A therapist specializing in fertility-related stress and neurodivergent support
5. Communicate with Your IVF Team
Be transparent about your PMDD symptoms with your fertility clinic. If you are experiencing PMDD symptoms while trying to conceive or while considering fertility treatment, your condition needs to be managed very carefully.
The Bottom Line
PMDD is a serious medical condition that affects millions of women worldwide. This staggering figure is a wake-up call, underscoring the urgent need for enhanced diagnostic processes, effective treatment plans, and robust support systems for those affected.
While PMDD doesn't directly cause infertility, it can significantly impact your IVF experience and treatment outcomes. The hormonal fluctuations inherent in fertility treatment may exacerbate PMDD symptoms, potentially affecting your mental health, treatment adherence, and overall well-being during this critical time.
By identifying and addressing PMDD before starting IVF, you're not just managing a condition—you're optimizing your chances for treatment success and protecting your mental health throughout the process. Remember, seeking help for PMDD isn't a sign of weakness; it's a crucial step in taking control of your fertility journey.
If you're experiencing severe mood symptoms or having thoughts of self-harm, please reach out for help immediately. Contact your healthcare provider, call 000, or go to your nearest emergency room.
References
Johns Hopkins Medicine. (2025). Premenstrual Dysphoric Disorder (PMDD). Available at: https://www.hopkinsmedicine.org/health/conditions-and-diseases/premenstrual-dysphoric-disorder-pmdd
Cleveland Clinic. (2023). Premenstrual Dysphoric Disorder (PMDD): Causes & Treatment. Available at: https://my.clevelandclinic.org/health/diseases/9132-premenstrual-dysphoric-disorder-pmdd
Mishra, S., Elliott, H., & Marwaha, R. (2023). Premenstrual Dysphoric Disorder. StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK532307/
Islas-Preciado, D., Ramos-Lira, L., & Estrada-Camarena, E. (2025). Unveiling the burden of premenstrual dysphoric disorder: a narrative review to call for gender perspective and intersectional approaches. Frontiers in Psychiatry, 15, 1458114.
Reilly, T. J., et al. (2024). The prevalence of premenstrual dysphoric disorder: Systematic review and meta-analysis. Journal of Affective Disorders, 349, 534-540.
University of Oxford. (2024). New data shows prevalence of Premenstrual Dysphoric Disorder. Available at: https://www.ox.ac.uk/news/2024-01-30-new-data-shows-prevalence-premenstrual-dysphoric-disorder
Schmidt, P. J., et al. (2017). Premenstrual Dysphoric Disorder Symptoms Following Ovarian Suppression: Triggered by Change in Ovarian Steroid Levels But Not Continuous Stable Levels. American Journal of Psychiatry, 174(10), 980-989.
IVI Fertility. (2025). Does Premenstrual Dysphoric Disorder Affect Fertility? Available at: https://www.ivi.uk/blog/premenstrual-dysphoric-disorder-pmdd-does-it-affect-fertility/
Broughton, T., Lambert, E., Wertz, J., & Agnew-Blais, J. (2025). Increased risk of provisional premenstrual dysphoric disorder (PMDD) among females with attention-deficit hyperactivity disorder (ADHD): cross-sectional survey study. British Journal of Psychiatry, 226(6), 410-417.
Lin, P. C., Long, C. Y., Ko, C. H., & Yen, J. Y. (2024). Comorbid Attention Deficit Hyperactivity Disorder in Women with Premenstrual Dysphoric Disorder. Journal of Women's Health, 33(9), 1267-1275.
Various sources from medical journals and institutions documenting the relationship between PMDD, ADHD, and autism as cited throughout the text.
